The Future of Personalized Cancer Vaccines: Transforming Oncology with Precision Immunotherapy

Photo by Iván DÃaz on Unsplash
Introduction: A New Era in Cancer Therapy
Personalized cancer vaccines are rapidly reshaping the landscape of cancer treatment, offering hope for more precise, effective, and less toxic therapies. Unlike traditional approaches, these vaccines are tailored to each patient’s unique tumor profile, aiming to train the immune system to recognize and eradicate cancer cells while sparing healthy tissue. Recent clinical breakthroughs, technological innovations, and evolving regulatory pathways have positioned personalized cancer vaccines as a cornerstone of future oncology care. This article explores the latest advances, practical pathways for accessing these therapies, and what patients, clinicians, and advocates can expect in the coming years.
Breakthrough Clinical Progress and Real-World Results
In the past two years, RNA-based and neoantigen-targeted cancer vaccines have achieved unprecedented validation in clinical trials, particularly for difficult-to-treat cancers such as melanoma, pancreatic cancer, and glioblastoma. For example, the NeoVax MI vaccine, developed by Dana-Farber Cancer Institute, has demonstrated that modifying vaccine formulation and delivery can significantly enhance immune responses in advanced melanoma patients. The phase 1 trial showed that updated vaccine strategies are not only feasible and safe but also generate a more powerful and specific immune response than previous versions. These results underscore the critical importance of ongoing innovation in vaccine design and administration [3] .
Moreover, over 120 active clinical trials are currently testing various personalized cancer vaccines, marking the most coordinated and ambitious development effort in the history of cancer immunotherapy. The anticipation of the first commercial approvals by 2029 is realistic, given the robust clinical pipelines and regulatory momentum [1] .
How Personalized Cancer Vaccines Work
Personalized cancer vaccines are designed by identifying unique genetic alterations-called neoantigens -within a patient’s tumor. Using advanced sequencing technologies and bioinformatics, scientists analyze tumor tissue to pinpoint these abnormalities. The selected neoantigens are then synthesized into vaccine components, which are administered to stimulate the patient’s immune system to recognize and attack cancer cells displaying these markers, while leaving normal cells unharmed [4] .
The process typically involves:

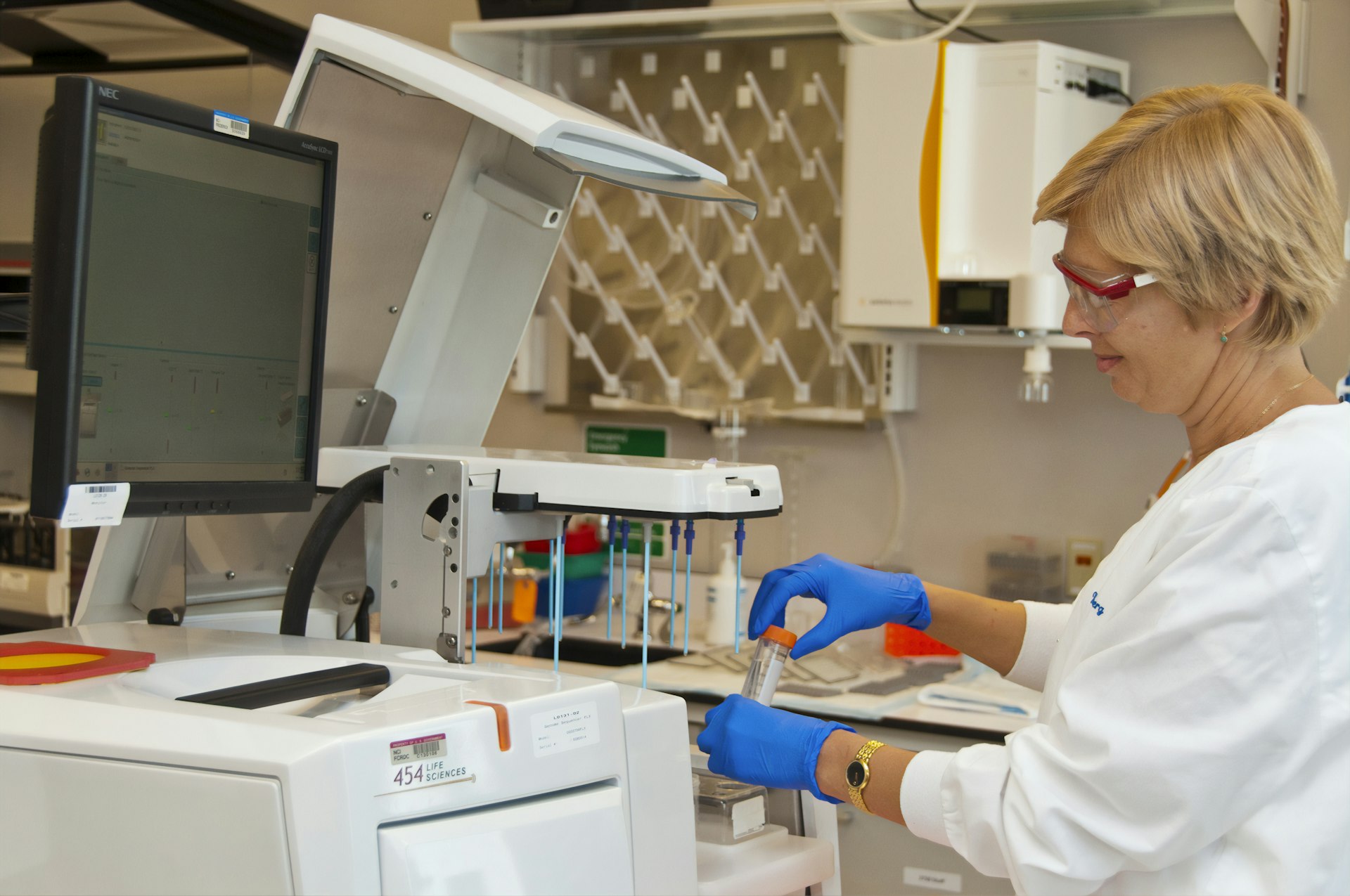
Photo by camera obscura on Unsplash
- Biopsy and sequencing: A sample of the patient’s tumor is obtained and analyzed with next-generation sequencing to identify mutations unique to their cancer.
- Neoantigen identification: Computational tools prioritize which mutations are most likely to trigger an immune response.
- Vaccine design and manufacturing: The neoantigen peptides or mRNA sequences are synthesized and formulated into a vaccine.
- Administration and monitoring: The vaccine is delivered to the patient, often alongside immune-boosting adjuvants, and immune responses are carefully tracked.
This highly individualized process aims to maximize specificity, reduce side effects, and address the challenge of tumor heterogeneity.
Technological Innovations Driving the Future
Several technological advances are accelerating the development and effectiveness of personalized cancer vaccines:
- Layered nanoparticle delivery systems: These help improve vaccine stability, targeting, and uptake by immune cells, enhancing efficacy [1] .
- CRISPR-enhanced platforms: Gene editing tools like CRISPR are enabling more precise identification and targeting of cancer mutations.
- AI-guided vaccine design: Artificial intelligence and machine learning streamline mutation analysis, neoantigen selection, and predict immunogenicity, resulting in faster and more effective personalized vaccine development [5] .
- Advanced sequencing and bioinformatics: Next-generation sequencing (NGS) platforms and advanced computational tools are key to identifying a broader and more actionable range of tumor mutations [2] .
These innovations are reducing production timelines, improving vaccine specificity, and making personalized approaches feasible even for rare or complex cancer types.
Combination Therapies and Clinical Strategies
Personalized cancer vaccines are increasingly being combined with other immunotherapies to enhance their effectiveness. Pairing neoantigen vaccines with immune checkpoint inhibitors (such as PD-1 blockers) or adoptive T-cell therapies (like CAR-T cells) has shown the potential to overcome immune suppression within the tumor microenvironment. For example, combining personalized vaccines with PD-1 inhibitors has already produced enhanced immune responses and improved outcomes in cancers such as melanoma and non-small cell lung cancer [2] .
These combination strategies are likely to become standard practice as our understanding of the immune system and tumor biology deepens. They offer hope for patients whose cancers have previously resisted conventional treatments.
Regulatory Pathways and Access
Regulatory agencies like the U.S. Food and Drug Administration (FDA) and their international counterparts have taken significant steps to support the accelerated development of personalized cancer vaccines. Comprehensive guidance and harmonized international standards are streamlining the approval process, making it more feasible for new vaccines to reach patients quickly [1] .
However, these therapies remain largely available through clinical trials. To participate or get more information, patients and providers can:
- Consult with their oncologist about eligibility for ongoing clinical trials involving personalized cancer vaccines.
- Search the National Cancer Institute (NCI) or clinicaltrials.gov for “personalized cancer vaccine” or “neoantigen vaccine” trials relevant to their cancer type and location.
- Contact major cancer centers, such as Dana-Farber Cancer Institute or University of Arizona Health Sciences, to inquire about current research protocols and referral pathways.
It is important to note that commercial approvals may be possible by 2029, but access outside of clinical trials is currently limited. Manufacturing advances and global access initiatives are being developed to reduce costs and support broader distribution in the future [1] .
Challenges and Solutions
Despite rapid progress, several challenges remain for the widespread adoption of personalized cancer vaccines:
- Cost and Manufacturing: Custom design and production for each patient currently result in high costs. Manufacturing decentralization and technology transfer to regional centers may help reduce expenses over time [1] .
- Equity and Access: Global access initiatives aim to ensure these therapies are not limited to well-resourced centers or countries. Partnerships between academic centers, governments, and industry can help expand reach.
- Scientific Complexity: Personalized vaccine development requires interdisciplinary expertise in genomics, immunology, and bioinformatics. Ongoing training and collaboration are essential to scale these approaches.
Alternative strategies, such as off-the-shelf vaccines targeting common cancer mutations, are also in development but may offer less specificity than fully personalized approaches. Patients should discuss all available treatment options with their care team.
How to Access Personalized Cancer Vaccine Trials and Resources
If you or a loved one is interested in pursuing personalized cancer vaccines, consider the following steps:
- Speak with your oncologist about the potential suitability for vaccine-based immunotherapy and request a referral to a major cancer center involved in this research.
- Search for active clinical trials using official resources such as clinicaltrials.gov or the National Cancer Institute’s website. Use search terms like “personalized cancer vaccine,” “neoantigen vaccine,” or the specific cancer type.
- Contact research institutions such as Dana-Farber Cancer Institute, University of Arizona Health Sciences, or other leading academic cancer centers to learn about ongoing trials and eligibility criteria. Visit their official websites or call their clinical research offices for the most accurate information.
- Consider joining patient advocacy groups or cancer support organizations that can provide updates on emerging therapies and clinical trial opportunities.
Eligibility for trials is typically based on cancer type, stage, previous treatments, and specific genetic markers. Participation generally involves tumor biopsy, genetic sequencing, and frequent monitoring.
Be aware that personalized cancer vaccine therapy is an evolving field, and availability may change as new studies are launched and therapies receive regulatory approval. Always rely on guidance from trusted medical professionals and official research channels.
Looking Ahead: The Road to Mainstream Adoption
The future of personalized cancer vaccines is bright, with robust scientific momentum and growing clinical evidence supporting their transformative potential. As technology advances, costs decline, and global access improves, these therapies may soon become widely available, offering new hope for patients with challenging or treatment-resistant cancers. Ongoing collaboration between researchers, clinicians, regulators, and patient advocates will be essential to fulfill the promise of precision immunotherapy in oncology.
References
- [1] Magoola, M. et al. (2025). Current Progress and Future Perspectives of RNA-Based Cancer Vaccines. PMC. RNA-based cancer vaccines achieve clinical validation and technological breakthroughs.
- [2] Singh, P. et al. (2025). Advancements and challenges in personalized neoantigen-based cancer vaccines. Frontiers in Oncology Reviews. Explores future directions and combination strategies for neoantigen vaccines.
- [3] Dana-Farber Cancer Institute (2025). Modified Personalized Cancer Vaccine Generates Powerful Immune Response. Reports on the NeoVax MI clinical trial in melanoma.
- [4] University of Arizona Health Sciences (2025). Developing the personalized future of cancer treatment. Details efforts to create neoantigen-specific vaccines.
- [5] American Association for Cancer Research (2025). Experts Forecast Cancer Research and Treatment Advances in 2025. Discusses the integration of AI and new vaccine modalities.
MORE FROM cheerdeal.com