Navigating the Future of Telehealth: Trends, Innovations, and Access in the Post-Pandemic Era

Photo by Kingsley Nguyen on Unsplash
Introduction: The Evolving Role of Telehealth
Telehealth has undergone a dramatic transformation since the onset of the COVID-19 pandemic. What was once an alternative has rapidly become a central pillar of healthcare delivery, offering expanded access, convenience, and efficiency. As we move deeper into the post-pandemic era, telehealth continues to evolve, integrating new technologies and care models to meet the changing needs of both patients and providers. This article explores the future of telehealth, offering guidance on how individuals and organizations can access and benefit from these advancements while addressing emerging challenges and opportunities.
Key Trends Shaping Telehealth in the Post-Pandemic Era
1. Artificial Intelligence (AI) and Automation
AI is revolutionizing telehealth by enhancing diagnostics, automating patient triage, and streamlining administrative tasks. AI-powered chatbots now provide 24/7 support, answer routine questions, and schedule appointments, allowing providers to focus on more complex cases. Predictive analytics are being used to anticipate health risks and personalize care strategies, while AI tools in diagnostics and imaging reduce human error and support earlier interventions for better patient outcomes [1] . For example, AI chatbots can collect symptoms and triage queries before a patient even meets with a provider, making interactions more efficient [5] .
To access these advancements, patients can look for healthcare providers who advertise AI-enhanced telehealth services or ask during virtual consultations about the use of AI tools in their care process. Providers interested in adopting AI should research established telehealth platforms that offer built-in AI capabilities and ensure staff are trained on their use.
2. Hybrid Care Models: Blending Virtual and In-Person Services
Hybrid care models-combining telehealth with traditional face-to-face visits-are now widely preferred by patients and clinicians. Surveys indicate that more than 80% of both groups support these models, reflecting a desire for flexibility and comprehensive care [2] . Hybrid models allow patients to access consultations, follow-ups, and chronic disease management remotely while reserving in-person visits for procedures or complex assessments.
Patients interested in hybrid options should check with their insurance providers or local clinics to understand which services are available virtually and how to coordinate between telehealth and in-person care. Healthcare organizations can implement hybrid models by integrating telehealth platforms with existing practice management systems and providing clear communication channels for patients to choose their preferred mode of care.
3. Specialist Access and Cross-Border Collaboration
Telehealth breaks down geographical barriers, enabling patients to access specialists who may not be available locally. This is especially valuable in regions facing provider shortages or for rare conditions requiring expertise not found nearby. Health systems are increasingly sharing specialist resources, and cross-border telemedicine is expanding, allowing for international consultations and second opinions [3] , [5] .
To leverage this, patients may seek referrals from their primary care physicians or search for telehealth networks specializing in remote consultations. Many major hospital systems now offer virtual specialty care; patients can inquire with their provider or conduct an online search for “national telehealth specialty clinics.” Healthcare professionals can join telehealth networks to expand their reach and collaborate with peers globally.
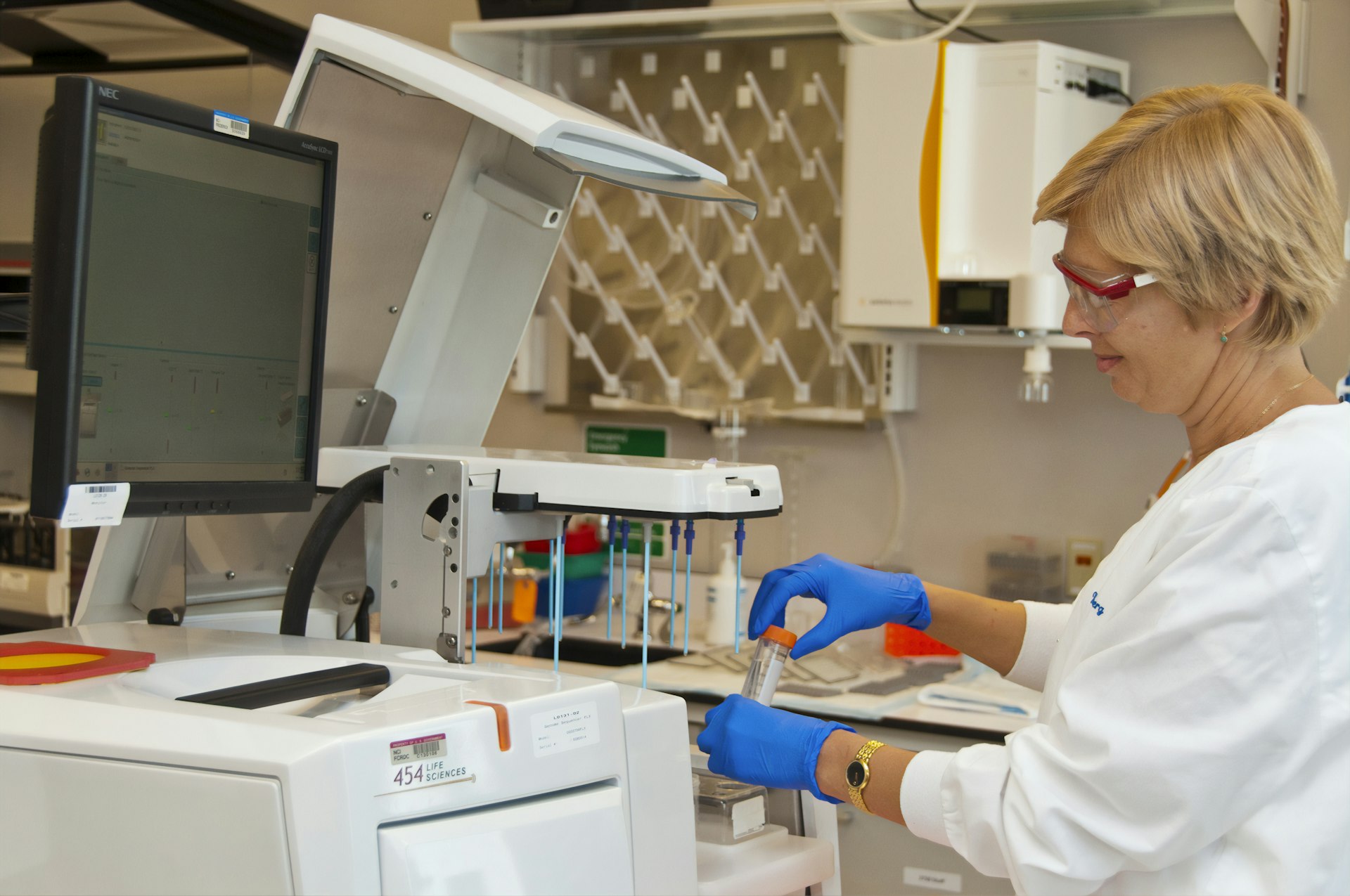
4. Technological Advancements: Remote Monitoring, Wearables, and Robotic Procedures
Remote patient monitoring (RPM) and wearable devices are becoming integral to chronic disease management. These tools collect real-time health data-such as blood pressure, glucose, or heart rate-which is transmitted to providers for ongoing oversight and early intervention. Wearables empower patients to take a more active role in their health while supporting timely clinical decisions [1] , [5] .

Photo by engin akyurt on Unsplash
For more acute needs, robotic-assisted procedures and “hospital at home” models are expanding, enabling some surgeries or advanced care to be delivered remotely or in the patient’s home environment. To access RPM or wearable-based care, patients should speak with their primary care team about eligibility and device options. Many insurance plans cover certain RPM services; patients can verify coverage by contacting their provider or insurer directly.
5. Data Interoperability and Digital Health Records
Enhanced interoperability between Electronic Health Records (EHR) systems is a top priority. Improved data sharing means less duplication, seamless transitions of care, and more accurate, up-to-date patient records across providers and settings [5] . Secure APIs and IoT devices are facilitating better integration, although challenges in standardization and privacy remain.
If you are a patient, you can request that your healthcare providers share and update your digital health records across different facilities. To ensure privacy, inquire about your provider’s data security protocols. Healthcare administrators looking to improve interoperability should consider EHR vendors with proven track records and compliance with established standards like HL7 and FHIR.
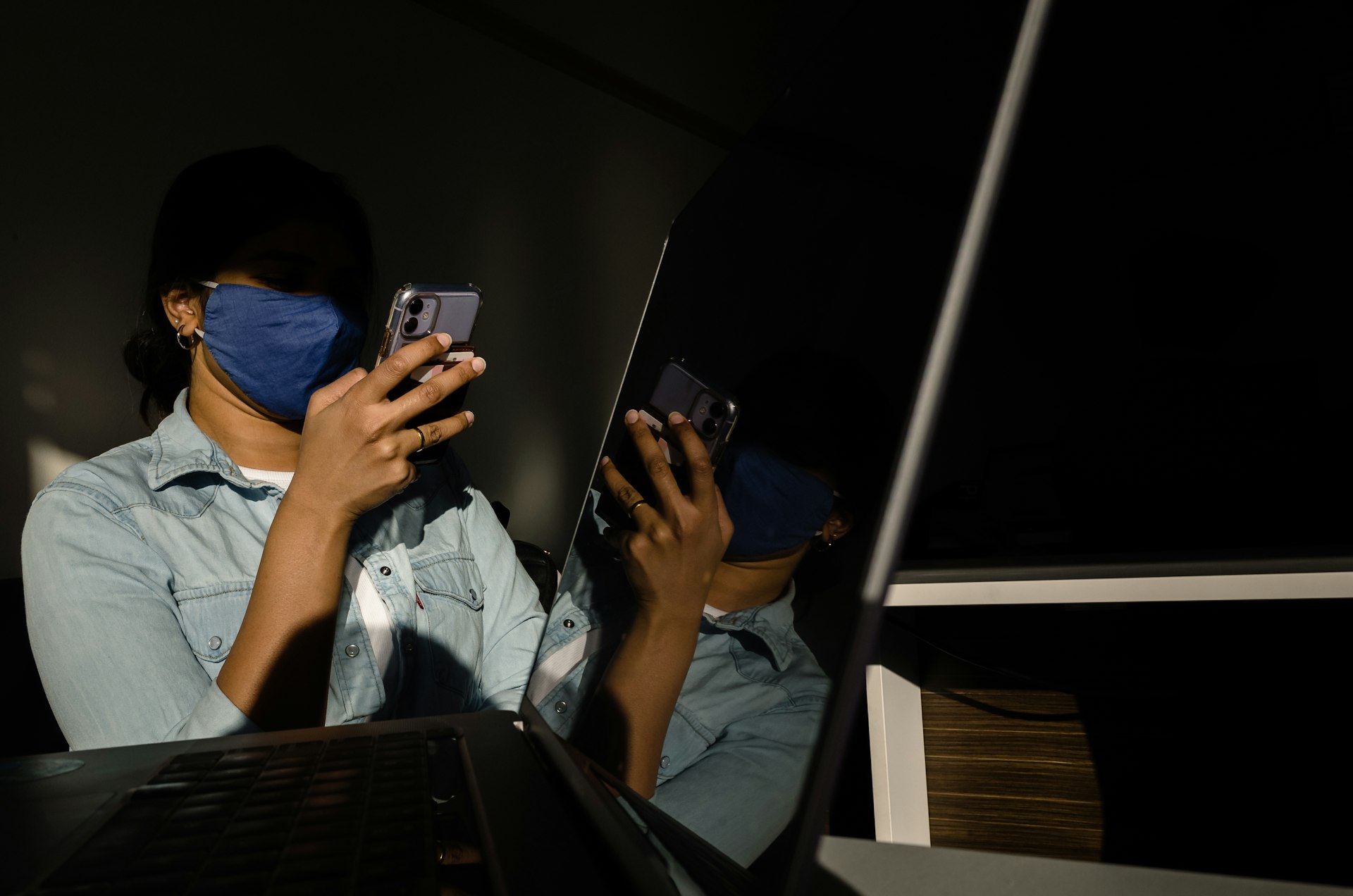
Addressing Challenges: Equity, Accessibility, and Security
While telehealth offers unprecedented opportunities, challenges persist. Access to high-speed internet, digital literacy gaps, and insurance disparities may hinder some populations, especially in rural or underserved communities. Organizations are working to close these gaps through device loan programs, patient education, and partnerships with community organizations [4] .
Security and privacy are also key concerns. As telehealth platforms collect more personal health information, robust cybersecurity measures and ongoing user training are essential. Patients should use only secure, reputable telehealth platforms and avoid sharing sensitive information on unencrypted channels. Providers must ensure compliance with privacy regulations, such as HIPAA in the United States, and regularly update security protocols.
Practical Steps to Access and Benefit from Telehealth
For Patients:
- Consult Your Primary Care Provider: Ask about available telehealth options for consultations, follow-ups, or chronic care management.
- Check Insurance Coverage: Contact your health plan to verify which telehealth services are covered and whether copays apply.
- Prepare for Virtual Visits: Ensure you have a stable internet connection and a device with audio/video capabilities. Test your setup before appointments.
- Explore Remote Monitoring: For chronic conditions, request information on RPM devices and how data will be shared with your care team.
- Prioritize Security: Use only official telehealth platforms recommended by your provider and never share passwords or sensitive details via email or text.
For Healthcare Providers:
- Integrate Telehealth Platforms: Choose platforms compliant with privacy laws and capable of connecting with your EHR system.
- Train Staff: Invest in telehealth-specific training, including best practices for virtual communication and troubleshooting technical issues.
- Communicate Clearly: Provide patients with instructions for accessing virtual appointments and support for technical issues.
- Monitor Regulatory Updates: Stay informed about evolving telehealth regulations, licensure requirements, and reimbursement policies from agencies such as the Centers for Medicare & Medicaid Services (CMS).
Alternative Pathways and Future Directions
Many community health centers, hospital systems, and private practices are expanding telehealth offerings. If your usual provider does not offer telehealth, search for “virtual care clinics” or “telemedicine providers” in your state. For those without reliable internet access, public libraries, community centers, or local telehealth hubs may offer secure spaces and connectivity for virtual visits. Advocacy groups are working to expand broadband access and digital literacy, and patients can reach out to local health departments for assistance.
Looking ahead, telehealth is expected to further integrate with wearable technology, leverage advanced AI for personalized care, and become more deeply embedded in routine healthcare delivery. Regulatory frameworks will likely continue to evolve, with a focus on ensuring equitable access, privacy, and high-quality outcomes [4] .
Summary: Key Takeaways for Patients and Providers
The future of telehealth is dynamic, technology-driven, and focused on delivering equitable, high-quality care. By staying informed of new advancements, proactively seeking out telehealth services, and advocating for accessible options, patients and providers alike can benefit from this ongoing transformation. Whether through hybrid care models, AI-powered tools, or improved data integration, telehealth is poised to be a primary avenue for healthcare delivery for years to come.
References
- [1] Emerline (2025). Telehealth Trends 2025: Key Insights Into the Future of Virtual Care.
- [2] National Rural Health Association (2025). 5 Telemedicine Trends for Hospital Leaders in 2025.
- [3] CHG Healthcare (2025). Trends in Telehealth: The Future of Virtual Care.
- [4] Dimensional Insight (2025). The State of Telehealth in 2025.
- [5] Sermo (2025). Future of Telemedicine: Top 20 Trends Shaping Healthcare in 2025.
MORE FROM cheerdeal.com