How Biomechanics Transforms Injury Rehabilitation: Science, Technology, and Step-by-Step Recovery

Photo by Rick Rothenberg on Unsplash
Introduction
The science of biomechanics -the study of movement mechanics in the human body-has become a cornerstone of modern injury rehabilitation. By analyzing how forces, motion, and neuromuscular factors interact during recovery, clinicians can design evidence-based strategies that restore function, prevent reinjury, and maximize patient outcomes. This article explores the impact of biomechanics on injury rehabilitation, presents actionable guidance, and highlights emerging technologies shaping the future of recovery.
The Role of Biomechanics in Injury Rehabilitation
Biomechanics provides a framework to understand how injuries alter movement patterns, muscle function, and joint stability. Rehabilitation specialists use biomechanical principles to identify movement deficits and tailor interventions for optimal healing. For example, after anterior cruciate ligament (ACL) reconstruction, biomechanical analysis helps clinicians assess muscle strength, joint stability, and compensatory patterns. Research has shown that selecting a hamstring-tendon graft can offer more balanced recovery in terms of muscle strength and knee stability compared to other graft types, guiding clinicians in making individualized treatment decisions [1] . Similarly, evidence-based strategies, such as targeted hip abductor strengthening combined with manual therapy or shockwave treatments, have proven effective for common running injuries like iliotibial-band syndrome, enabling faster and safer return to sport [3] .
Biomechanics and Neuroplasticity: Preventing Reinjury
Recent research highlights the interplay between biomechanics and neuroplasticity -the brain’s ability to adapt after injury. Advanced rehabilitation approaches now consider how the brain and body work together to relearn movement, reduce compensations, and prevent reinjury. Dustin Grooms and his team at Ohio University’s OMNI institute have found that incorporating neurocognitive training can optimize recovery by retraining the brain and body simultaneously, benefiting athletes, military personnel, and everyday patients [2] .
To implement these strategies, rehabilitation may include:
- Virtual reality -based perceptual-motor exercises to retrain movement patterns
- Markerless motion capture to monitor progress and detect subtle deficits
- Cognitive-motor tasks that challenge both brain and body coordination
Patients should consult with physical therapists who specialize in neuro-biomechanical rehabilitation and inquire about programs that integrate these technologies.
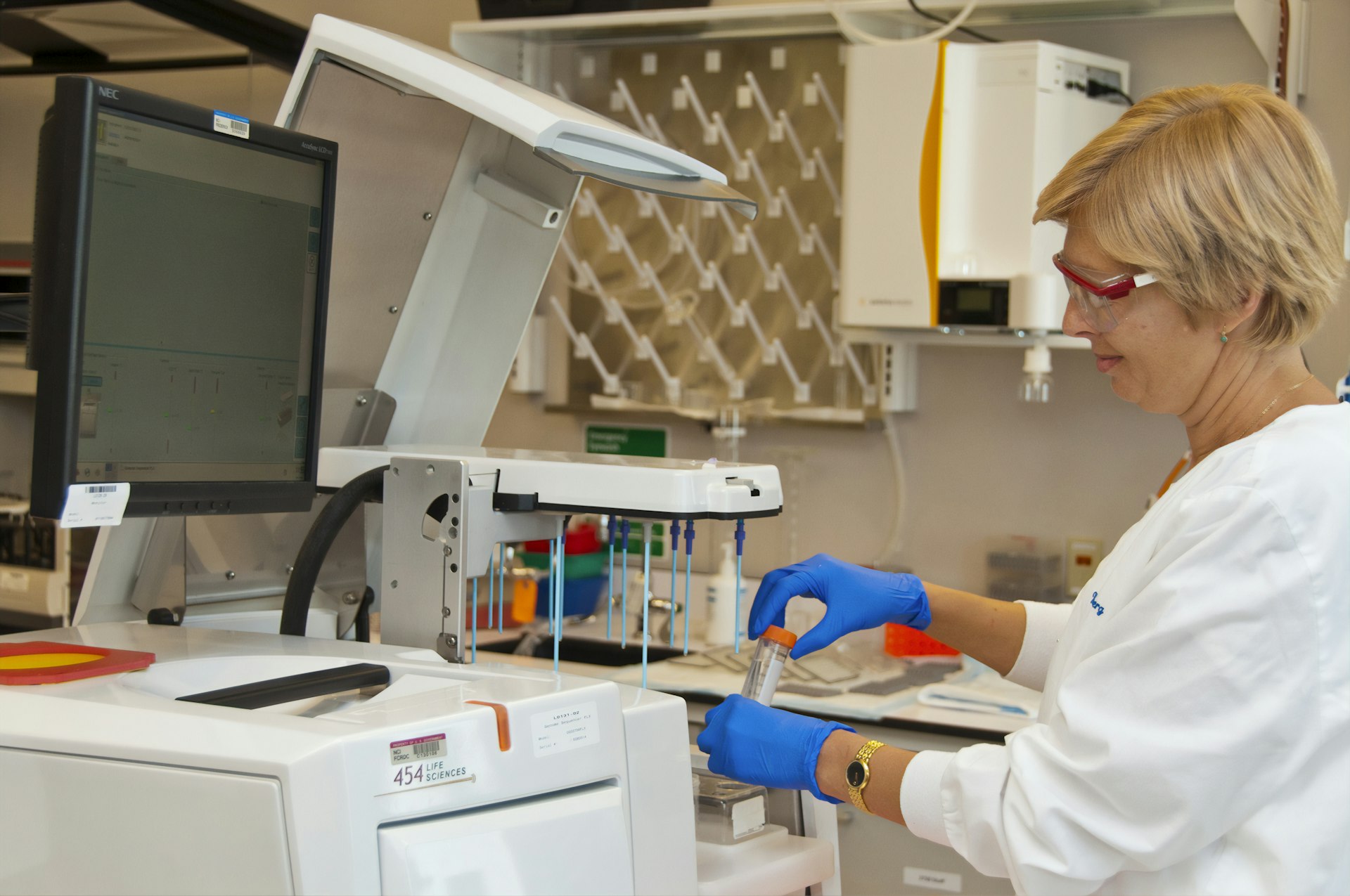
Emerging Technologies and Methodologies
Technology is rapidly transforming biomechanics-driven rehabilitation. Markerless motion capture systems now allow clinicians to analyze movement without cumbersome equipment, providing reliable data on kinematics and force profiles [1] . Instrumented-mouthguards are being used to monitor head impacts and inform safer return-to-play protocols in contact sports [3] .
To access these services:
- Consider rehabilitation centers affiliated with research universities, such as Ohio University’s OMNI Institute or the Musculoskeletal Biomechanics & Rehabilitation program at USC, which utilize advanced motion analysis and neurocognitive training [4] .
- Ask your provider about technology-assisted assessment tools-such as wearable sensors or motion capture-for personalized feedback.
Step-by-Step Guidance for Implementing Biomechanics-Based Rehabilitation
To maximize the benefits of biomechanics in your recovery, follow these steps:
- Seek a Comprehensive Movement Assessment: Schedule an evaluation with a physical therapist or rehabilitation specialist trained in biomechanical analysis. They will use observation, wearable sensors, or motion capture to assess your movement strategies, muscle activation, and joint function.
- Understand Your Individual Movement Deficits: The assessment will identify compensatory patterns, weakness, or instability unique to your injury. For example, after ACL surgery, you may have quadriceps weakness or altered gait mechanics that require targeted intervention [1] .
- Develop a Personalized Rehabilitation Plan: Work with your provider to design an evidence-based program. This may include muscle strengthening, neuromotor retraining, flexibility exercises, and sport-specific drills. For runners with iliotibial-band syndrome, hip abductor strengthening is key [3] .
- Incorporate Neurocognitive Training: Ask about integrating virtual reality, dual-task exercises, or perceptual-motor drills to retrain both your brain and body for better movement control and injury resilience [2] .
- Monitor Progress and Adjust Interventions: Regularly reassess your biomechanics using motion analysis or wearable technology. Adjust your program as needed for continued improvements.
- Educate Yourself and Advocate for Advanced Care: Stay informed about new technologies and research. If your rehabilitation provider does not offer advanced biomechanical assessment, request referrals or search for programs at major academic centers, such as USC or Ohio University [4] .
Real-World Examples and Case Studies
Biomechanics-driven rehabilitation has produced measurable improvements in diverse patient populations:
- ACL-reconstructed athletes who received personalized biomechanical assessment and targeted strength training recovered muscle balance and returned to sport with lower reinjury risk [1] .
- Runners with iliotibial-band syndrome who participated in hip abductor strengthening and manual therapy reported reduced pain and improved function, facilitating safe return to running [3] .
- Children with cerebral palsy benefited from technology-assisted neuromotor rehabilitation, improving their ability to plan and execute movement [5] .
Potential Challenges and Solutions
Challenges in biomechanics-based rehabilitation include access to advanced technology, cost, and provider expertise. To navigate these issues:

Photo by Yucel Moran on Unsplash
- Contact major academic medical centers or university-affiliated rehabilitation programs, which often offer cutting-edge biomechanical assessment and research-driven care.
- If technology is unavailable, request thorough observational movement analysis and inquire about evidence-based exercise protocols.
- Discuss insurance coverage and potential out-of-pocket costs for advanced assessment tools.
Some individuals may experience variability in recovery due to physiological, technical, or motivational factors. Personalized programs and ongoing assessment help address these differences [1] .
Alternative Approaches and Additional Resources
If you do not have access to high-tech rehab centers, consider these alternatives:
- Search for certified physical therapists in your area who use biomechanical assessment and evidence-based protocols. Use trusted directories such as the American Physical Therapy Association (APTA).
- Ask about home-based movement analysis options, such as video gait analysis or app-based feedback tools.
- Contact local hospitals and inquire if they partner with university research teams for biomechanics-driven rehabilitation studies.
For more information, you can visit the official websites of leading research centers, such as the USC Musculoskeletal Biomechanics & Rehabilitation program [4] or the Children’s Hospital of Philadelphia for pediatric rehabilitation research [5] .
Summary and Key Takeaways
Biomechanics is revolutionizing injury rehabilitation by enabling precise assessments, evidence-based interventions, and integration of neurocognitive strategies. Personalized care, advanced technology, and ongoing research are making it possible to restore function, prevent reinjury, and improve quality of life for diverse patient populations. Individuals seeking the best outcomes should pursue comprehensive movement assessment, evidence-based rehabilitation plans, and stay informed about the latest advancements.
References
- [1] Frontiers in Sports and Active Living (2025). Advancing biomechanics: enhancing sports performance and rehabilitation.
- [2] Ohio University News (2024). Preventing reinjury: How neuroplasticity and biomechanics are changing injury recovery.
- [3] National Institutes of Health PMC (2025). Advancing biomechanics: enhancing sports performance and rehabilitation.
- [4] University of Southern California (USC): Musculoskeletal Biomechanics & Rehabilitation.
- [5] Children’s Hospital of Philadelphia (CHOP): Injury Rehab and Biomechanics Engineering Research.
MORE FROM cheerdeal.com